After a challenging workout, the last thing you probably want to do is spend five to 10 minutes stretching, but doing so can result in much-needed physical and mental health benefits. But why is stretching important and how often do you need to do it?
“Stretching helps keep us mobile. We are born super mobile as babies and young children, but lose this as we grow into adults,” “When we stop stretching, we lose capacity in movement. Decreased capacity in movement means we are able to move less; we are functionally less able to do everyday stuff like pick up a pen from the floor, scratch our back, or even climb stairs efficiently.”
Why stretching is good for your body
“When you think about exercise, most people participate in some type of aerobic activity that improves their cardiovascular endurance. Most people are doing weight training to help maintain lean muscle mass and to build strength, These are two very important elements of a fitness program, but there’s also a third element, and that is your flexibility and mobility, which is most often the one that’s neglected.
With certain stretches, like yoga or tai chi, it’s taking you in a more relaxed state. It will help to decompress and bring your stress level down and get you in a better frame of mind.”
Additional health benefits of stretching include:
- increased blood flow to the brain and throughout the body
- increased flexibility and range of motion
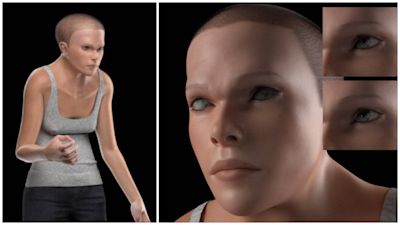
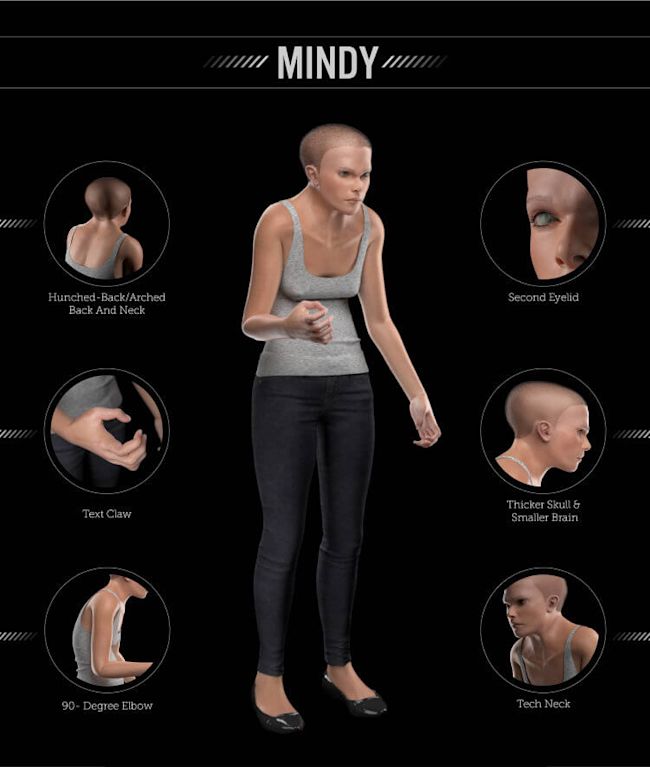
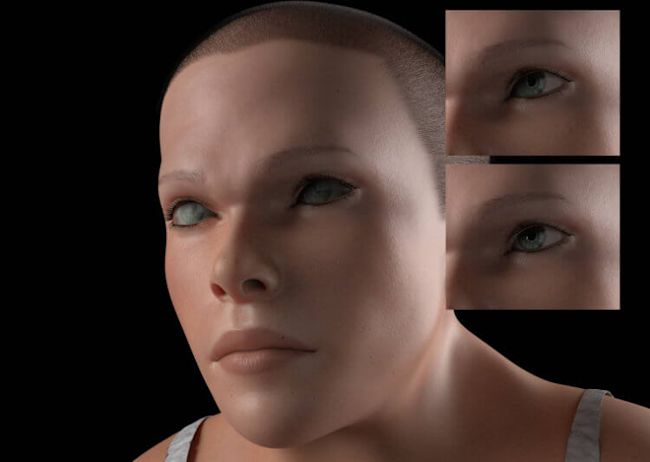
- improved posture
- improved athletic performance
- relief from back pain and tension
- helps prevent injuries
Stretching is going to help with physical and mental relaxation and relieve muscle tension and soreness. It’s also going to help reduce the risk of injury.
Some people are naturally more flexible than others, but no matter whether you can touch your toes or you’re barely able to get your hands halfway down to your shins, you should be working on your flexibility and mobility because the more sedentary you are, the more your muscles are shortening, which in turn is causing you to be more tight.
Stretching is good for your brain
In addition to helping feel relaxed, stretching increases your body’s levels of serotonin, which is the hormone that can help stabilize your mood and reduce stress. Studies found that implementing stretching exercises at work also reduced anxiety and exhaustion while increasing vitality and mental health.
Add stretching to your everyday routine
There are two main types of stretching: static stretching, where you hold a stretch for a certain amount of time, typically between 15 and 30 seconds; and dynamic stretching, which incorporates more functional movements. But you’ll want to make sure you’re properly warmed up before stretching so as not to injure yourself. When any particular restriction is causing issues a gentle but 90 seconds stretch can aid the fascia and tendons to return long lost flexibility. However this is time consuming so we recommend only one or two areas per day
“Dynamic stretching is moving through a range of motion to help prep muscles and ligaments for performance and should be done before workouts,”