There has never been a better time to focus on getting rid of those aches and pains.
There has never been a better time to focus on getting rid of those aches and pains.

As we slowly move back into normality it is important not to forget our health and well-being. Lockdown allowed us time to reflect and take more care of our bodies. Let’s not waste all this effort.
Many people are suffering from the effects of increased laptop usage in poor workstation spaces at home. Stiff necks, headaches, shoulder pain and low back discomfort are the major complaints at the moment.
Lots of us have developed overuse injuries from excessive exercises such as running daily or too many kettlebell workout sessions.
Maybe a good time for a general checkup with
theOsteopath.
Take care of yourselves all.

Welcome to theOsteopath.net http://theosteopath.net/


Osteopaths provide safe, effective treatment and care that aims to promote the health of patients. Using manual therapy, health advice and sometimes exercise, tailored to the needs of the individual, people of all ages see osteopaths, from babies to the elderly.
Osteopaths are highly trained healthcare professionals, with expertise in the musculoskeletal (MSK) system – that is the muscles, joints and associated tissues and their relationship with other systems of the body.
People who visit an osteopath consistently report high satisfaction with the care they receive1, expressing high confidence in the treatment and advice of their osteopath2, with rates in excess of 90% for both satisfaction and trust.
They also work closely with other healthcare professionals such as consultants, GPs, nurses, midwives, physiotherapists.

To find your nearest osteopath please visit our Find an Osteopath page.
Osteopaths will use a wide variety of gentle hands-on techniques that focus on releasing tension, improving mobility and optimising function, together with providing useful health advice and exercise if required.
They will also work with, or refer you to, other healthcare professionals as needed to ensure you receive optimum care. They take the time to understand each patient – your unique combination of symptoms, medical history and lifestyle. This helps to make an accurate diagnosis of the cause of your issue, (not just addressing the site of discomfort), and formulate a treatment plan with you that will achieve the best outcome.

People commonly visit osteopaths for MSK conditions, such as back, neck, joint, muscle and arthritic discomfort. Osteopaths have a well-deserved, evidence-based reputation for expertise in the treatment of these conditions.
People also visit osteopaths for a variety of other health reasons including neuromuscular conditions such as sciatica, digestive issues, headaches and migraine prevention. To find out more about how osteopaths can help, please click here.
Most osteopaths work in local private healthcare clinics and you can visit them without the need for a GP referral.
To find your nearest osteopath please visit our Find an Osteopath page.

Osteopaths are regulated by law and recognised as an allied health profession by NHS England. This gives them a similar status to dentists or physiotherapists and guarantees the equivalent high level of care.
By law, an osteopath must be registered with the General Osteopathic Council (GOsC) to practise in the UK.
Before an osteopath can obtain registration, they must attain specialist degree-level training, either a Bachelor of Science (BSc.) or integrated Masters (MOst.), plus complete over 1000 hours of clinical placements (direct patient contact time).
To maintain their registration with GOsC, which is renewed annually, osteopaths must meet mandatory continuous professional development (CPD): keeping skills and knowledge up-to-date and maintaining high standards of professional development.
When visiting an osteopath for the first time, it is natural to feel a little unsure of what to expect. The following information explains what happens and answers any questions you may have.
The iO is the professional membership organisation for osteopaths. We represent over two-thirds of registered UK osteopaths in the UK. Our members operate in line with the iO Patient Charter, the values and purpose of which demonstrates their commitment to providing the highest quality service and care to their patients.
We hope that you have found this information useful. If you haven’t yet arranged an appointment with an osteopath – you can search for one in your area using here or by telephoning 01582 488455.
Latest News from The Migraine Trust
Source: A new migraine landscape
|
|
|
|
|

OPHM is a new not-for-profit special interest group within osteopathy.
At the core of OPHM is a group of experienced osteopaths working nationwide.
Each of us has a long-standing special interest in headaches which we would like to share with other osteopaths wishing to increase their knowledge and skills in headache management.
Correct diagnosis of subsections of Migraine and headache is very important. There are hundreds of varieties which are listed in The International Classification of Headache Disorders. Members of OPHM have experience in assessing Headaches and identifying many of these and also treating many of the physical triggers.
For more information on Headaches and Migraines visit our webpages.
Call/ Text 07841576335 or email david@theosteopath.net for an appointment
Source: Cervicogenic Headache: Diagnosis and Management
Cervicogenic headache constitutes 15 to 20% of all chronic and/or recurrent headaches and is categorized as a secondary headache, meaning the condition results from an underlying disease. CGH specifically stems from a neuromusculoskeletal dysfunction of the cervical spine, particularly the upper three cervical segments.1,2,3
The World Cervicogenic Headache Society has defined CGH as head pain that is referred from a primary nociceptive source in the musculoskeletal tissues innervated by the cervical nerves.4 It is characterized by a unilateral headache with signs and symptoms of neck involvement, such as pain on movement, by external pressure over the cervical spinal segments, and/or sustained awkward head postures.5,6,7 The differential diagnosis for CGH is wide and includes, in part: migraine, occipital neuralgia, arteriovenous malformation, Chiari malformation, meningitis, glaucoma, pseudotumor cerebri, vasculitis (especially temporal arteritis), cervical spondylosis, tumor, and autoimmune conditions including rheumatoid arthritis and vertebral artery dissection.8
Broadly speaking, the literature has a wide range as to the definition and diagnostic criteria of this disorder. For instance, several sources exclude arthritic conditions, spondylolisthesis, or other disorders associated with aging of the upper cervical spine that are not attributable to the development of CGH. As a result, CGH may be characterized by headache resulting from non-arthritic conditions of the cervical spine and has been shown to occur during the manipulation or stimulation of the upper cervical spinal segments.
One source suggests that CGH usually presents clinically as a hemicranial pain syndrome caused by upper cervical spine disorders of the three spinal nerves. In addition, dysfunctions of structures that are innervated by these nerves may be possible sources of the headache.9 Pain often involves the posterior occipital area of the skull and extends to the ipsilateral orbit. The upper three cervical nerve roots associated include: the infra-tentorial dural membranes and branches of the trigeminal (V1) supra-tentorial membranes.10 In evaluating post-neurosurgical pain, Kemp, et al, discussed the innervation of the dura in the posterior cranial fossa.11
Several schemes have established the general diagnostic criteria of CGH as the reproduction of the headache following stimulation of the upper cervical nerve roots. In addition, anesthetic blockade is widely regarded as a confirmatory test, although often considered unnecessary in clinical diagnosis.5,6,7 This approach connects this syndrome to dysfunctional upper cervical neural structures. As a result, the underlying cause of cervical neurologic dysfunction must be established. Film radiographs, magnetic resonance imaging (MRI), and computed tomography (CT) myelography appear to have limited use in diagnosing CGH.7 MRI evaluation of the cervical spine “reported no demonstrable differences” between CGH patients and a control group in the appearance of cervical spine structures on MRI scans.7 Diagnosis is made by clinical presentation and diagnostic criteria, and may only be definitely confirmed by stimulation of upper cervical nerve roots.12
The physiologic basis of upper cervical dysfunction leading to CGH is known to lie in the convergence of the afferent branches of trigeminal nerve (fifth cranial nerve) with the upper three cervical sensory nerves, called the trigeminocervical complex (TGC).13 These converging signals excite the spinal cord interneurons, which relay outputs to local structures and ascend to the thalamus and sensory cortex. Depending on the duration and severity of the original sensory input, the TGC may be susceptible to hyperexcitability, which may lead to hypertonic muscles and pain in structures that share this innervation. Further, TGC may also affect the parasympathetic (vagus) and sympathetic systems impacting diverse functions in the chest, head, and face.8 When pain and hypertonicity resustain, neuroplastic changes may occur at the spinal cord level where minimal provocation elicits an exaggerated response, or central sensitization.14
Pharmacological management of cervicogenic headache typically involves utilization of:
Additional treatment modalities may include:
Within the literature, manual medicine—which seeks to restore upper cervical mobility through a wide range of therapeutic procedures, including mobilization and manipulative techniques—has been found beneficial in CGH as well. Several studies have identified benefit regardless of gender, age, or headache chronicity.16,17 Manual restoration of upper cervical and thoracic spinal mobility to reduce peripheral input is one of the main objectives for the successful treatment of CGH.18 A review of random controlled trials involving manual therapy, including OMT, showed statistically significant improvement in patients’ symptoms, especially when combined with exercise.19
Consistent with current understanding of CGH, “osteopathic physicians theorize that cervical mobilization and manipulation procedures decrease the afferent stimulus into the spinal cord from cervical joint receptors by relaxing the paraspinal muscles and releasing strain on the connective tissues and joints, thus relieving the pain of CGH.”8 An osteopathic approach to CGH may be beneficial therapeutically, but also diagnostically. As noted, imaging studies and other diagnostic modalities are often of limited value beyond evaluating the differential diagnosis of CGH. In addition, the reproduction of CGH symptoms with nerve stimulation has demonstrated consistency in diagnosis across medical and therapeutic paradigms.
A central component in the osteopathic approach to patient evaluation and treatment always includes a thorough history and physical exam supported by an in-depth understanding of the underlying anatomy and physiology. If abnormal findings are identified through traditional clinical skills or palpation, appropriate testing and treatment is implemented immediately. In the absence of “alarm symptoms,” addressing the condition from an osteopathic perspective involves looking at the whole body, with specific attention to each of the areas involved in the pathogenesis of CGH, including the upper cervical spine; the cervical musculature and ligaments; and the cranial and jaw structures.
In most cases, reduced range of motion (ROM) and pain represent the function of the “sensitized” cervical output with hypertonicity and pain in CGH. An osteopathic physician may utilize specific diagnostic procedures and criteria to identify the presence of somatic dysfunctions in the region of interest. The presence of somatic dysfunction may indicate disturbances in associated nerve roots; in the muscular, fascial, and ligamentous structures; as well as in the local autonomic and lymphatic functions.8 With CGH, cervical somatic dysfunction typically affects not only the perception of pain, but also the physiologic and nociceptive function of any shared innervated organ and skeletal structures.8 Essentially, the identification of somatic dysfunction is a physical manifestation that a segment is sensitized. While any area of the body may result in cervical spine dysfunction, one of the most important causes of CGH may be myofascial trigger point activity, specifically from the sternocleidomastoid muscles.20,21
Once identified, appropriate OMT may be used to treat the somatic dysfunction, which may, in turn, resolve CGH symptoms. Specifically, OMT may help to restore homeostasis as evidenced by improved ROM, reduce pain in the spinal and cranial nerve structures, and reduce swelling and inflammation. OMT methods may address soft tissue, counterstrain, fascial release, muscle energy, and high velocity/low amplitude. The type of OMT applied in CGH treatment depends on the tolerance of the patient and the specific diagnostic findings.
Chronic headaches affect a sizeable portion of the population and present a significant cost to the healthcare system. Evaluations suggest that many clinicians order unnecessary testing, such as imaging; delay treatment of pain by referring to sub-specialists; or utilize non-specific pharmacotherapy in managing pain.22
Secondary cervicogenic headache, in particular, is amenable to diagnosis and treatment without imaging, sub-specialist referral, or the use of medications that tend to reduce symptoms rather than treat the disorder. An osteopathic approach, including osteopathic manipulative treatment, may be well suited for both the evaluation and treatment of CGH. When OMT is utilized appropriately, patients with CGH may find relief and resolution of their symptoms while minimizing additional imaging and medication costs.
For an initial appointment to assess Cervicogenic headaches call
07841576335 or email david@theosteopath.net
This article was published as an online exclusive in association with the June 2019 issue of PPM.
Stretching Everyday
Why do I need to Stretch?
In today’s world the nature of our lifestyle is much less active. We have, over the last few years become much more sedentary.
This is mainly due to the advances in technology. Sitting becomes the most commonly performed action. We no longer need to stand up and take down files or even go to the fax and copy machines. We do it all on our PC and more than ever our smart phones.
When we sit with our knees bent, the three hamstring muscles relax, they attach on our ‘sit bones’ (ischial tuberosities) and partly the back of the Femur. At the other end they attach below the inside and outside of the knee. They are, in essence a postural muscle responsible for controlling the strong quadriceps on the front of our legs. They need to remain in a state of constant readiness, called resting tone. If shortened for any length of time, small receptors in the muscles called ‘muscle spindles’ measure their length, send messages via the spinal cord to the cerebellum to reduce the resting tone length.
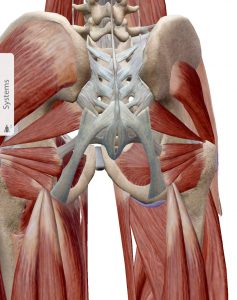
This is why after being seated for any length of time at a desk or in a car, plane, train or sofa, the act of standing become difficult as the muscles have become shortened. Stretching helps to re-set the resting tone to be longer again and also improve speeds and stride length when training.
Does Stretching Help?
Many patients ask about the benefits of stretching and whether or not it may help with their back problems. We will attempt here to explain the various benefits and disadvantages to be aware of within yourself, that may make Stretching part of your daily activities.
Recommended Daily stretches
Hamstrings, Hip Flexors, Gluteals, Calves, Neck muscles. For more details visit the following five pages on differing body areas for stretching.
Other muscles commonly shortened
In the side of the neck when holding the telephone for long calls regularly, ladies check out the raised muscles when trying on that nice summer dress that always slips of the shoulder. The back of the neck when slouching on your chair gazing at the lap top or screen that is too far away from you. A classic for developing that headache that comes on later in the day! Those Psoas or Hip flexors that attach fom the inside of your upper leg, head through the and under your tummy vessels to a fix to the front of the lumbar veterbrae, when you stand up they are tight and create a bigger dip in your low back, this can make your tummy look larger and bloated. Wearing High Heals shortens the calf muscles making wearing flat sandal painful in the achilles tendon.
Is it wise to see an Osteopath before starting regular stretches?
Probably a good thing as the osteopath will be able to assess the quality of the muscles and their respective functions. This allows the osteopath to advise which stretches are more beneficial and specific to you and the environment you are in.
The Osteopath
When visiting an Osteopath with chronic or acute problems, you are assessed and treated with a view to prevention of further injury, combined with corrective exercise. The Osteopath is empathetic to the patient’s need to establish a speedy recovery of the body and return to the achievement of intended goals.
Today at the World Migraine Summit we watched an excellent interview with Dr. Vincent Martin MD.

Some enlightening answers to the following questions. His research can be found on PubMed.
The reduction in Oestragen being a major trigger along with decrease barometric pressure with precipitation for some or increase for others. Pressure changes in the cranial cavity and fluid if the brain are well known triggers. Hence headaches post Spinal tap. As Osteopaths here we spend a great deal of treatment time reducing the structural causes acting on this area.
• Why are migraine symptoms sometimes misconstrued as migraine triggers?
• Why does susceptibility to a trigger vary from day to day?
• How can menstrual migraine be prevented?
• What are repetition and avoidance theories, and how do they relate to managing triggers?
• Is there a migraine app that is best for determining whether a trigger is truly a trigger?
• What can be done to prevent migraine with barometric pressure changes?
• How can we manage odor and noise sensitivity in everyday life?
• How can the light sensitivity trigger be better managed?
• Does trigger sensitivity get worse with age?
Dr Vince Martin, MD is Director and Headache Specialist at the University of Cincinnati Headache and Facial Pain Center
He is the leading authority on weather and migraine. After graduating from the University of Cincinnati College of Medicine, Dr. Martin completed a residency in internal medicine, followed by a fellowship in general internal medicine at UC. He is currently director of the Headache and Facial Pain Center at the University of Cincinnati Gardner Neuroscience Institute, and has been professor of clinical medicine in the division of General Internal Medicine at the University of Cincinnati College of Medicine since 2004. Dr. Martin is president of the Ohio Headache Association and the National Headache Foundation, and is also a fellow of the American Headache Society and the American College of Physicians.
Spent a good 35 mins watching Dr. Robert Cowan at the Migraine World Summit, discussing why the lack of training causes a great deal of misdiagnoses of Migraines. They are doing some very interesting search with Artificial Intelligence which may well be groundbreaking. Anyone with Headaches and Migraines can contribute on the website http://www.bontriage.com. They also have a useful app that can be downloaded from the website.
Dr. Robert Cowan is a professor of neurology and director of the Headache and Facial Pain Program at Stanford University. He is board-certified in neurology and pain medicine with a subspecialty certification in headache medicine. Dr. Cowan holds several nationally elected positions, including chair of the section on chronic daily headache for the American Headache Society.
He is President of the Headache Cooperative of the Pacific and a fellow of both the American Academy of Neurology and the American Headache Society. He sits on the board of the Alliance for Headache Diseases Advocacy and the American Headache and Migraine Association. He has published over 50 articles and is the author of The Keeler Migraine Method.
A Groundbreaking, Individualized Treatment Program from the Renowned Headache Clinic Paperback by Robert Cowan
More than 30 million people suffer from debilitating headaches. Yet our understanding of the science behind migraines is still in its in-fancy. At the Keeler Center for the Study of Headache, Dr. Robert Cowan and his team of specialists conduct some of the most cutting-edge research in the field. Their treatment program, which combines the latest alternative and conventional therapy strategies, has helped thousands of sufferers manage their symptoms effectively and regain control of their lives.
As Dr. Cowan explains, each patient presents unique sets of triggers and pain patterns and requires a customized treatment approach. The Keeler method helps migraine sufferers identify their own headache triggers and then create an individualized formula for dramatically decreasing the frequency and severity of these attacks. It also illustrates how to design a foolproof, reliable ?rescue? plan when necessary, and offers surprising information, such as:
· Why elimination diets and ?foods to avoid? lists may not work
· Why frequently prescribed medications can actually make a headache worse
· Why many headache treatments stop working over Time